A professor of palliative care and member of the House of Lords has claimed that while palliative care in Malta shows considerable promise, it remains in its early stages.
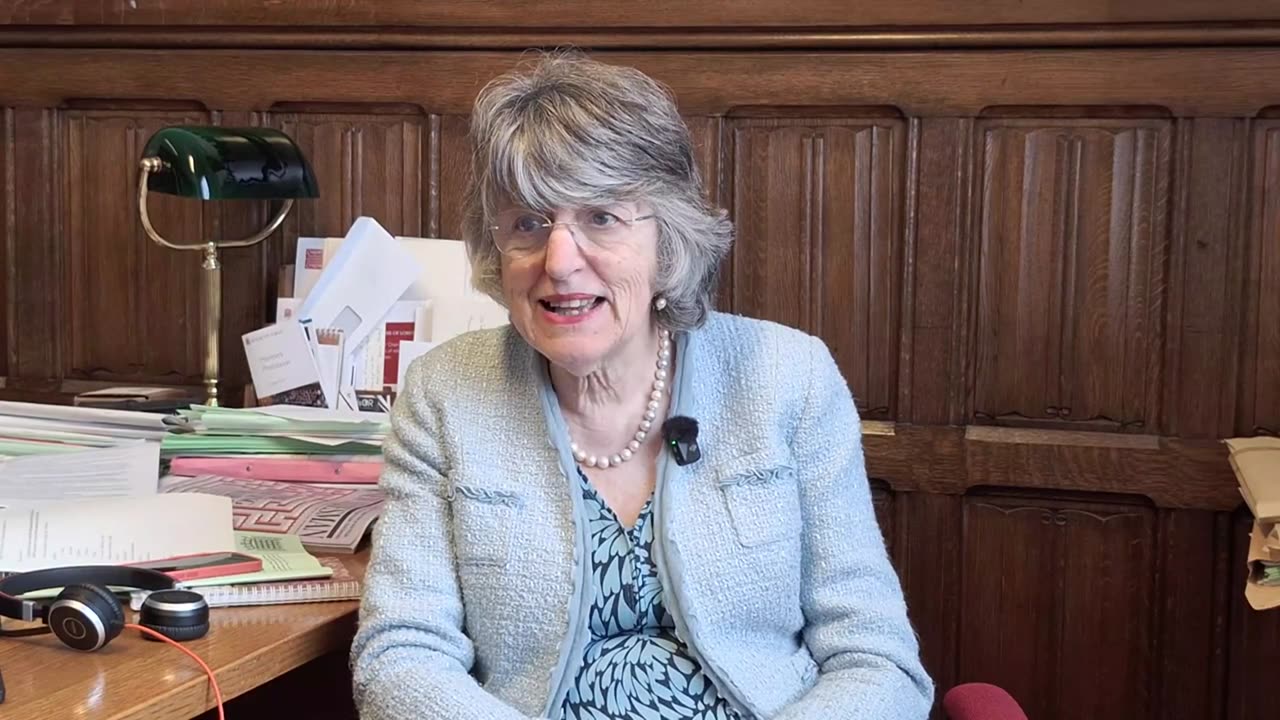
In an exclusive interview with Newsbook Malta at the Palace of Westminster in London, Professor Ilora Finlay expressed concern at the limited number of professionals in Malta specialising in palliative care. According to her, the number is so low that they could be counted on one hand. Despite this, she praised their dedication and their ongoing efforts to improve the quality of care.
Professor Finlay, who has decades of experience in the field, warned that if legislation on assisted suicide and euthanasia is introduced, progress in palliative care will be significantly hindered.
On 7 May, the Maltese Government launched a public consultation on the principles and so-called safeguards for the introduction of voluntary assisted euthanasia. The consultation process is scheduled to close on 2 July.
Professor Finlay commended the work of Maltese professionals in the field, noting that although they are few in number, they are deeply motivated to advance this form of care.
When palliative care services develop as they should, Professor Finlay noted, there is less waste in other areas of care.
This happens because unnecessary interventions are avoided and the care is tailored more closely to the patient’s real needs, she added.
Palliative care, Professor Finlay explained, focuses on the whole person. By addressing each patient’s individual needs, it provides timely support that allows people with terminal illnesses to maintain independence for as long as possible.
She shared examples from her practice, including a patient with a neurological disease who, although unable to move, continued to run a multinational business from bed using speech-assisted technology. Another patient, who was close to death, expressed a wish to complete a book he had been writing. The team arranged for a secretary to transcribe his words, and he was able to fulfil a lifelong ambition before passing away.
This should be the work we invest in, she added.
She also noted that good palliative care can reduce healthcare costs. On average, it has been shown to save around £1,700 (approximately €2,000) per patient. This is achieved by providing care that is specific to individual needs and by avoiding the waste of resources on unnecessary interventions.
Professor Finlay acknowledged the dedication of Malta’s small palliative care workforce but pointed out a serious gap in education. Unfortunately, Professor Finlay said, this treatment is not being taught in medical schools and it is something that is only being taught at postgraduate level, but it needs to be taught at all educational levels for those interested in the medical field.
‘Safeguards do not exist… these are vague conditions’
Professor Finlay also voiced concern over the safeguards proposed in euthanasia laws. Based on her experience, she stated that such provisions often amount to vague conditions rather than true safeguards.
In every euthanasia legislation I have seen, they are no longer called safeguards but vague conditions, she said.
While some criteria – such as age – are straightforward to verify, other conditions lack clarity and certainty.
The consultation document released by the Maltese Government states that to qualify for euthanasia, a specialist in the patient’s medical field must certify that the condition is irreversible and terminal, with the patient unlikely to live more than six months.
Professor Finlay warned that it is impossible to provide such assessments accurately if the patient is not receiving proper care. She also questioned how any system could effectively detect whether pressure is being placed on a patient to choose death prematurely.
‘Life is precious and we must protect it’
Over the course of her career, Professor Finlay has met many patients who felt that their lives were complete – yet still hoped to live a little longer for specific reasons.
Patients would be willing to stay alive for days or weeks to see their children return from a trip, only to give up and die peacefully, she said.
She recalled one case where, after weeks of careful effort from the palliative team, a man was able to see his daughter get married. He died two days later, but he had completed the last thing he wanted to do, Professor Finlay said.
It is unfortunate that there are those who die prematurely without having prepared a will, or without any warning to their relatives, in an accident, she said, adding that “we are all going to die. None of us will live forever, and we must stop pretending that we will live forever. Life is precious and we must protect it. We must accept that death comes to us all.”
In recent days, the Life Network Foundation launched a campaign titled Kill the pain, not me, advocating for better palliative care and opposing the legalisation of assisted suicide.
The campaign urges the public to engage with the government’s consultation via the platform oqtollugigh.org, encouraging people to stand up for natural end-of-life care. The submission process takes less than a minute and is intended to amplify public support for dignity in dying – without resorting to euthanasia.
Source: Newsbook.com.mt