A professor of palliative care and member of the House of Lords has shared the story of a terminally ill patient who, after receiving timely palliative treatment, went from being in acute pain and struggling to breathe to sitting up, pain-free and drinking tea, all within half an hour.
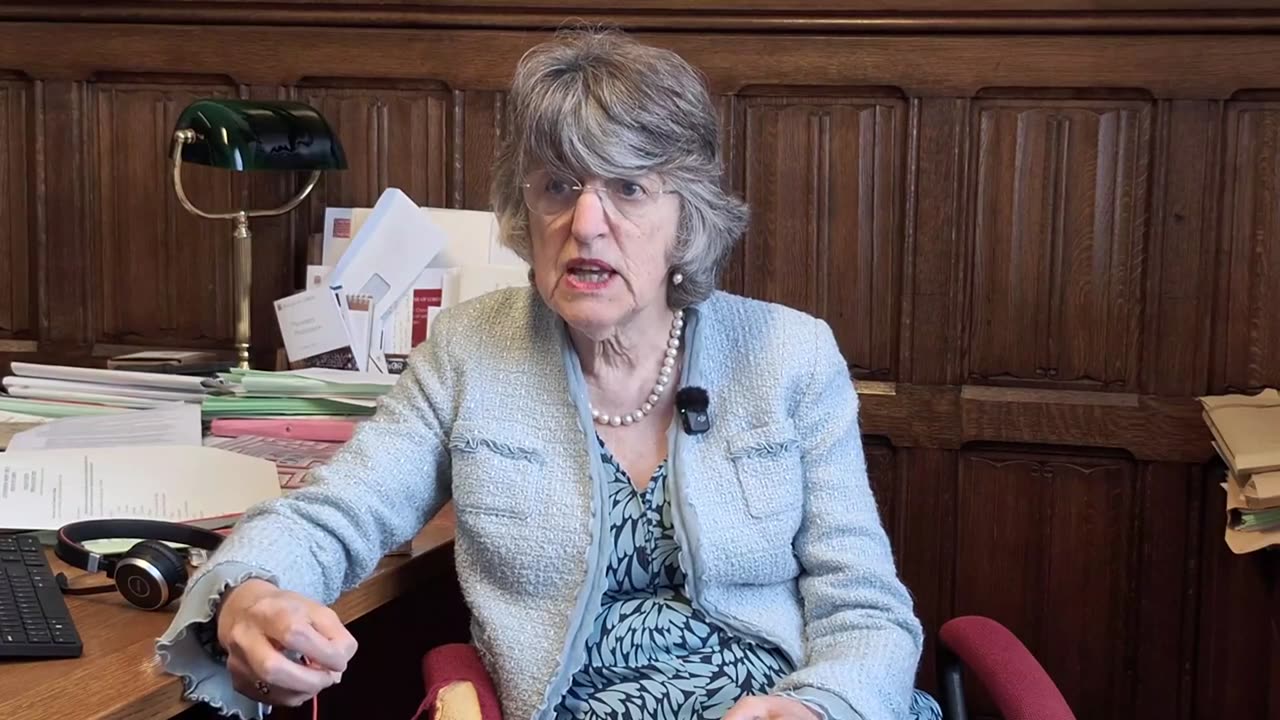
In an interview with Newsbook Malta at the Palace of Westminster, Professor Ilora Finlay recounted how the man’s family had approached her, requesting help to end his life. Instead, she administered appropriate palliative care, and within minutes, the patient’s condition had markedly improved.
Professor Finlay, who has worked in the field for decades, explained that palliative care treats the whole person, not just the medical condition. It considers the physical, emotional, and social needs of both patients and their families, offering dignity and comfort even in the face of death.
Whatever the problem – physical, emotional, or social – palliative care seeks to improve quality of life for as long as possible, she noted.
Although the UK has long debated euthanasia and assisted suicide, the discussion has intensified in recent years. In 2024, MP Kim Leadbeater tabled a motion proposing legislation to allow terminally ill adults in England and Wales to choose to end their lives.
The major political parties have not taken an official position, allowing MPs to vote according to conscience and constituents’ wishes. Notably, several MPs – including Jonathan Hinder and Rebecca Paul – are reportedly reconsidering their prior support and may now vote against the bill.
Professor Finlay said that part of the role of palliative care is to accept death as a natural process, neither hastened nor unnecessarily delayed.
In the case of the terminally ill man whose family had sought euthanasia, she recommended admission to a hospice. Within 30 minutes of assessment, she administered medication at the right dose and at the right time, relieving his pain and distress.
His wife began to cry when she saw that the situation could improve.
This is what should be done for every patient and no one should be led to believe that the only solution to suffering is to end their life, Professor Finlay said, adding that the answer to suffering is not to kill the patient, but to relieve them of their suffering.
If a healthcare professional does not know how to provide relief, Professor Finlay said, they have a moral and ethical duty to consult someone who does. Sometimes it only takes a phone call. She noted that she has received calls from all over the world – some involving cases that seemed insurmountable, but which often had simple solutions.
She underlined the importance of collaboration between doctors, oncologists, and other healthcare professionals, working together to improve quality of life for those who are suffering.
Ending a patient’s life is not a solution. Ending their suffering and keeping it under control is, she said.
Professor Finlay also addressed the fear patients often experience when they are left in the dark about their condition. Many worry about losing their cognitive abilities, or facing their final days without dignity. Palliative care, she explained, aims to maintain dignity in all aspects – not only medical, but also emotional and social.
She pointed out that dignity is shaped by how others treat you and if someone is treated as worthless, their dignity is diminished. But when a person in distress is asked how they are feeling and what can be done to ease their burden, their dignity is restored, Professor Finlay added.
Professor Finlay argued that the value of life is not dependent on ability or productivity. Rather, it is intrinsic. She criticised utilitarian philosophies for undermining the inherent worth of each human being.
Kill the pain, not me
In recent days, the Life Network Foundation launched a campaign titled Kill the pain, not me, advocating for better palliative care and opposing the legalisation of assisted suicide.
The campaign urges the public to engage with the government’s consultation via the platform oqtollugigh.org, encouraging people to stand up for natural end-of-life care. The submission process takes less than a minute and is intended to amplify public support for dignity in dying – without resorting to euthanasia.
Source: Newsbook.com.mt